Features of the extended semen analysis by the Kruger method
In order to assess the indicators of men's health, various tests are used. One of them is the study of sperm - the expanded spermogram according to Kruger.
What does the method show?
Extended Kruger spermogram is one of the methods for the diagnosis of reproductive pathologies. Most often, this method of research is assigned to future fathers, who for some reason have difficulty conceiving.
In this study, the morphological features of male germ cells (spermatozoa) are analyzed using special criteria - the Kruger scale. This study is not conducted by all men. There are certain medical indications for it. As a rule, reproductologists perform this laboratory test.
Strict morphology is achieved in the laboratory and helps to assess whether a woman can become pregnant by a particular man. Without careful study of the properties of male germ cells, this is impossible to achieve.
This research method was proposed by Professor Kruger at the end of the 20th century. He also developed and special indicators for which the evaluation. The method has been used for many years and allows doctors to obtain the necessary information about the existing pathologies of the reproductive health of men.
What is different from the usual semen?
The basic study of the ejaculate gives specialists only an approximate picture of the state of male reproductive health. In most cases, conducting this research method is sufficient. However, sometimes a more thorough analysis is required.
This question is especially “acute” if a man has any difficulties with conception. In such a situation, more advanced diagnostics are required. One of the prerequisites is evaluation of the morphology (structure) of male germ cells. This is possible thanks to the method of extended sperm according to Kruger.
Norms for natural pregnancy
In order for conception to occur, after all, many factors must "work". Very much also depends on the fertile health of a man.
The morphological structure of sperm is an important clinical feature that is necessary for the implementation of natural conception. The norm of sperm morphology is presented in the table below:
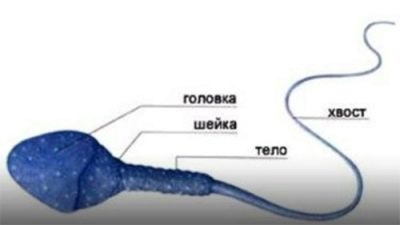
Assessed sign | Anatomical characteristic |
Head | Oval, slightly elongated. Length - 2.5 microns, width - 4 microns. |
Neck | It is a kind of transition from the head to the tail. Normal sizes should fit up to 1.5 of the head volume. |
Tail | Elongated shape, makes active movements. |
The structure (morphology) of the male germ cell is a very important criterion. For this, the ratio of the head, neck and tail of the spermatozoon is estimated. Normally, the head end is somewhat oval. Its tail is very mobile.
If morphological defects are not detected during the examination, this is an indicator of the norm. In this case, the possibility of merging with the egg increases.
Experts identify several pathological variants of the structure of the head of the male reproductive cell.Thus, it may have a pear-shaped, trapezoidal, conical and round shape. Other options are also possible, but they are extremely rare in medical practice.
There should be a direct connection between the head and the tail. If this "interaction" is violated, then it is a consequence of pathology. In such a situation, the trajectory of the sperm can also be broken.
Several years ago, doctors evaluated only the pathology of the anatomical shape of the head. All clinical parameters are currently being evaluated.
In conclusion, the study may be numbers. They indicate the number of affected sperm. So, if only the pathology of the head is present, then the number 1 is indicated. With the defeat of three anatomical parts (head, neck and tail) - number 3.
How to make a spermogram?
Before conducting a study, you should talk to your doctor so that he can prepare recommendations for preparing for the analysis. This type of examination can be taken in any medical institution that does such tests. Usually, studies are conducted in clinics where work is conducted with couples who have difficulty with the birth of a child.
In medical institutions, as a rule, there are separate rooms where a man can safely hand over his biomaterial. Modern clinics are trying to equip this room well, so that in it the representatives of the stronger sex were psychologically comfortable.
During the collection of biomaterial man no one bothers. Time is also usually not strictly regulated. For research going ejaculate. This is achieved by masturbation. The ejaculate is collected in a special container, which is given to a man before the analysis.
Proper preparation
In order for the results of the analysis to be qualitative and reliable, the examined man needs to be properly prepared. As a rule, in all medical institutions where such studies are conducted, there are special recommendations and instructions. They tell about what needs to be done for quality training before performing the survey.
Before going to the lab, a man is given complete sexual rest. This means not only stopping sex, but also prohibiting masturbation. This is necessary so that during the study the spermatozoa remain active and mobile.
Also, a few days before the survey, a man should not drink alcohol. Alcohol has an adverse effect on semen, which can lead to unreliable research results.
A couple of days before going to the laboratory for the delivery of biomaterial should limit the number of cigarettes smoked. Better on the day of the survey, the man does not smoke.
Exposure of too high temperatures to the body during preparation for the examination is also undesirable. Men who are planning to undergo such a study, a few days before the meeting should not visit the bath or sauna. In the summer and the hottest time, if possible, limit your stay in the active sun.
How is the transcript performed?
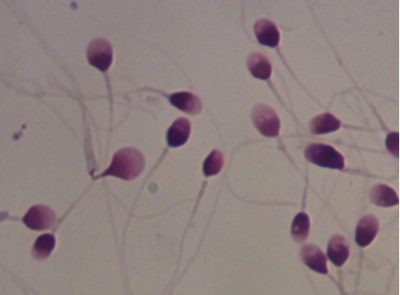
Conducted research in laboratory conditions, under the microscope. Subsequently, the "hands" issued a conclusion. All estimated clinical parameters obtained during the study are included in it.
It is impossible to establish the diagnosis by one analysis only. The result shows the presence of any functional changes, but is not a diagnosis.
In order to establish the pathology It is important to consult with several doctors. The examined man, as a rule, is advised by doctors of different specialties, including a fertility specialist and andrologist. These experts evaluate the results of the study and establish the diagnosis.
In a normal ejaculate there should be about 15,000,000 spermatozoa.If this content is substantially less, then we speak of two pathological conditions - “azoospermia” and “oligozoospermia”. They are unfavorable for further conception and require thorough medical correction.
In addition to quantitative counting, a qualitative analysis is also carried out. One of the estimated parameters is the vector of movement of male germ cells. Most of them should move in a straight line. This kind of biological movement is the most functional for the implementation of conception.
If the number of spermatozoa moving along such a trajectory is less than 32 percent, then this can be considered a pathological condition. It is called in medicine "asthenozoospermia".
Practically every member of the stronger sex has spermatozoa modified by morphological properties. This is normal: There is no 100% perfect sperm in shape and structure.
It is important to estimate the number of altered male germ cells. If there are too many of them, the possibility of natural conception is significantly reduced. This situation can make it extremely difficult for sperm to reach the female egg to fertilize it.
The pathology in which the morphological properties of male germ cells are significantly altered is called “teratozoospermia” in medicine. If this condition is pronounced strongly, the pair’s natural conception is significantly reduced. In such a situation, as a rule, one cannot do without appropriate treatment.
This advanced test also allows you to evaluate not only the functional and anatomical features of spermatozoa, but also to determine the basic properties of the ejaculate. So, you can also evaluate the viscosity, acidity, color and amount of biomaterial.
If a man had poor results with this examination, in this case, the doctor may refer him for a second test. Such a situation is also possible if the doctor has reasons to doubt the reliability of the obtained clinical data.
If during the examination of the man any pathological abnormalities were identified, a more advanced diagnosis is carried out. As a rule, many of the identified deviations contribute to a decrease in male fertility.
In order to clarify all possible violations and conducted auxiliary research. So, in this case, the doctor may recommend to be examined for specific ASAT (antisperm antibodies).
How to improve performance?
Often, some reasons and factors that are not permanent lead to a change in performance. For example, sperm counts in men who have just had colds or viral infections will be worse.
In this case, they should fully recover and recover, and only then undergo a similar study. It is better that between the acute temperature period and the delivery of the biomaterial to the study at least two weeks. The exact timing will tell the doctor after conducting a clinical examination.
High fever and fever have an adverse effect on sperm performance. However, after the cessation of their effects, the state gradually improves and returns to normal.
Antiviral drugs, as well as warm, abundant drinking will help restore the body more quickly. In the recovery period, you will also need funds that contain all the necessary vitamins and trace elements. They are appointed, as a rule, in the form of multivitamin complexes.
After complex treatment, repeated Kruger spermogram is best performed 6-8 weeks after recovery. In certain situations it may take more time.
Any inflammatory process contributes to the fact that in the ejaculate appear white cells - leukocytes.They are an important part of the immune system and are necessary to eliminate the infection.
The risk of leukocytes in the delivery of advanced analysis of the ejaculate - that they can lead to false results. In some cases, an inexperienced specialist conducting a study may simply take them for "inactive" sperm. Unfortunately, such cases still occur in medical practice.
For their minimization now in laboratories special dyes are used. They can be used to distinguish a white blood cell from a male germ cell. Doctors call such a laboratory test leucoscrinum. However, the human factor in the study can not be completely excluded.
In medical practice, there is also a special term. - Dunning-Kruger effect. It lies in the fact that specialists with low qualifications may make mistakes and even not recognize them.
If quite a lot of white blood cells were detected during the examination in the ejaculate, this may be a reason to re-conduct the study.
There should be enough time between re-surrender. At this time, the doctor must prescribe a man the appropriate treatment necessary to reduce the leukocytes in the semen.
The poor results of the study - this is not a sentence. It often happens that the modern way of life leads to their production. Constant stress, lack of sleep, irregular nutrition and other stimuli lead to the fact that a man’s health begins to deteriorate.
It is very important to follow him regularly. So, all men should definitely visit a urologist at least once a year.
If a man has any chronic diseases, they must also be treated on time. As a rule, the development of pathological changes in the spermogram can be prevented even by simple observance of a healthy lifestyle.
For the five steps that increase sperm motility naturally, see the following video.