All about cicatrix after cesarean section
Women who have undergone a cesarean section can easily bear and give birth to another, two, three or more children. True, the bearing of the fetus, its well-being, the possibility of giving birth on its own in the future, without the help of surgeons, predictions for the planning of a subsequent pregnancy directly depend on such a thing as a scar on the uterus. The scar remains, it is inevitable. In this article, we will describe how a scar is formed, what determines its viability or inconsistency, how to examine it and what are the norms for scar thickness.
How is it formed?
During caesarean section, the fetus and afterbirth are removed through an incision in the uterus. The incision can be vertical if the child needs to be removed as soon as possible (in some cases with an emergency CS) or horizontal in the lower segment of the uterus during a planned operation. After dissection, the edges in the incision area are tightened and sutured with special self-absorbable surgical sutures. A scar is formed at the dissection site from this point and for about 2 years.
Within a day after the operation of cesarean section, collagen bundles and fibrin threads lead to adhesion of the cut edges. At the sticking point, new myocytes start to form - uterine cells, small blood vessels are formed. A week later, elastic fibers appear, collagen is produced. The formation of new uterine cells is completed approximately three weeks after the operation. This is an ideal scenario, but in practice everything can be a little different.
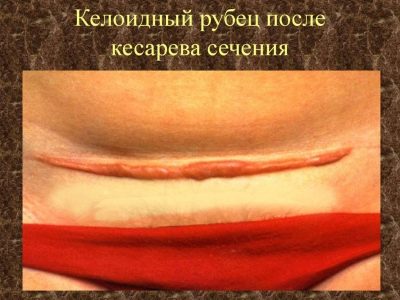
When exposed to negative factors, growth sites of hyalinized tissue are found among new myocytes. The proportion of coarse connective tissue prevails. Sometimes there are sclerotic processes around the formed blood vessels and in the neighboring tissues. This often leads to the formation of a pathological keloid scar.
It does not matter if it is longitudinal or transverse. Such a scar not only looks unattractive (this can be seen by doctors of diagnostics), but is also undesirable for planning pregnancy. The reasons for the formation of the scar comes with a predominance of connective coarse tissue, or the production of myocytes is insufficient, are numerous and not fully understood. It is believed that this process may be affected:
- postoperative complications, infections, inflammation;
- the state of the microflora of the genital tract of the puerperal;
- the general state of health of the woman before delivery;
- the place of the incision and the technique of imposing internal sutures, the skill of the surgeon.
It also increases the risk of insolvent scar formation in women, the causes of which are premature detachment of the placenta, its full presentation, a long anhydrous period, as well as severe preeclampsia, obesity and prolonged anemia. All these nuances after surgery lead to a state of temporary severe immunodeficiency crisis, which leads to improper healing of the incision site on the uterus.
Validity and failure - the rules
When a cesarean was a relative rarity, there was almost no question of the solvency or insolvency of the scar. Now the proportion of operative labor has increased, so the number of multiparous with a scar on the uterus is also about 15-20%.Despite these impressive figures, there is no single standard in Russia by which the scar could be considered wealthy or incomplete. While this question is left to the discretion of the doctor, and the opinions of doctors can be very different.
They are similar only in that the well-to-do need to consider a scar, which is homogeneous throughout its length, does not contain thinning, areas of pathological proliferation of connective tissue. In all other respects, the best medical minds of the planet have not yet come to a common opinion.
Russian scientists and practicing surgeons Lebedev and Strizhakov devoted several years to the clinical and morphological study of excised scar tissue, which they received during repeated operations of the CS. The result of their work is the following data on the allowable thickness of the scar in the norm:
Complete | Defective |
Thickness 4-5 mm | Thickness less than 3 mm |
Myometrium is defined clearly and along the entire length. | Myometrium is determined fragmentary or not defined. |
No local thinning | There are thinning, thickening, formation of keloid type |
The World Health Organization (WHO), relying on the results of European studies, argues that the minimum allowable thickness of a wealthy scar, in which even repeated natural births are possible (if only one caesarean section was done before) is 3.5 mm (from 36 to 38 weeks). The formation of a smaller thickness is not recommended as untenable, but independent delivery is undesirable.
In Canada, for example, it is common practice to measure the scar only for pregnant women who are going to give birth in a completely physiological way - through the birth canal. At week 38, a thickness of 2 mm is considered acceptable. And in Switzerland, 2.5 mm is considered an acceptable thickness before delivery. For non-pregnant women who are still thinking about the birth of another baby, in Russia, by default, it is considered to be a normal thickness of more than 2.5 mm. Anything less significantly increases the risk of uterine rupture, not only during contractions, but also long before them - during the carrying of the child.
Some diagnosticians are in full confidence that the thickness itself has little effect on the probability of rupture of the reproductive organ, it is the uniformity that is important along the entire length. This is indirectly confirmed by practice: sometimes women with a scar of 2 mm perfectly bear a child, who appears on time by repeated CS, and with a scar of 5 mm, but heterogeneous, serious problems arise.
It should be noted that any uterine scar increases the likelihood of a pathological pregnancy. Common pathologies due to scar are:
- miscarriage;
- infertility;
- fetal growth retardation;
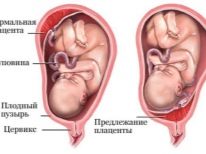
- placenta previa;
- the risk of early detachment of the "children's place";
- placental insufficiency;
- total ingrowth of the placenta into the cicatricial region may require the removal of the "baby site" along with the uterus.
The most dangerous is the rupture of the uterus. The genital organ grows with the baby, the uterine tissue is stretched, in the area of the collagen and myocyte scar less, and therefore the scar itself stretches very, very badly. Uterine rupture during pregnancy leads to severe internal bleeding, often - to the death of the mother and fetus. If the gap occurs in childbirth, there is a chance of salvation.
Diagnostics
With the diagnosis of the state of the scar in Russia and in the world, everything is not the best way. Hyperdiagnosis prevails when a doctor speaks to a woman with a good wealthy scar of 6 mm about the probability of rupture and persuades to have an abortion so as not to risk it. This is a completely understandable consequence of the lack of a unified standardization in determining the viability of scars.
Nevertheless, it is necessary to examine his condition. And it is desirable to begin this already 8-9 months after the operation. It is believed that it is precisely at this time that the scar “reveals” to the diagnostician all his “surprises”.In any case, before planning pregnancy, it is advisable to visit a doctor and insist on an examination of an internal suture on the uterus.
In the second half of pregnancy, it is recommended to recognize the thickness and structure of the scar at least once in 3 weeks, and in the last month - once in 10 days.
What diagnostic methods exist?
Ultrasound
This method is one of the most common, although its effectiveness for these purposes raises many questions in the professional community. Nevertheless, examination of the scar for consistency and the ability to withstand another pregnancy should begin with ultrasound diagnosis. Both transabdominal and transvaginal sensors are being examined. Indicators of intravaginal examination are considered more reliable.
The doctor will determine the length of the scar, be able to measure the thickness of the residual muscle layer, as well as determine the niche space under the scar. The doctor will declare an insolvent scar in the event that the niche is 50% or more in depth correlated with the residual muscle layer.
It is impossible to consider the results of ultrasound 100% reliable. Ultrasound diagnosis specialists themselves say that they make only a preliminary or auxiliary contribution to the diagnosis of scar tissue.
But to prohibit a woman to give birth or insist on abortion due to a thin scar according to the results of the ultrasound is clearly not worth it. More information on ultrasound about the state of the scar after cesarean can be obtained before pregnancy and in the first trimester. At the end of pregnancy, an adequate assessment is difficult.
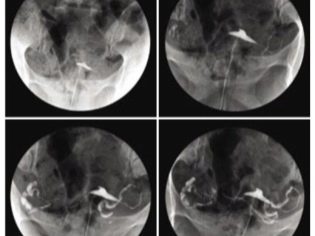
Hysterography
Quite an effective method of scar assessment, but with its own nuances. It is carried out only non-pregnant, since it implies contact with X-rays. In fact, the method is an x-ray of the uterus and its tubes using a contrast agent.
The procedure with an accuracy of up to 97% makes it possible to see signs of pathological scarring, but the method does not allow determining the true cause of what is happening and making predictions. For example, the diagnosis “endometriosis of a postoperative scar” on the basis of the X-ray picture obtained cannot be obtained, it is possible that an MRI scan of the uterus will be necessary. A slight displacement of the uterus forward according to the results of hysterography, roughness and jagged contours, defects in the filling of the uterus with a contrast solution can indicate an insolvent scar.
Hysteroscopy
This method also implies the absence of pregnancy at the time of the survey. An optical device (part of the hysteroscope) is inserted into the uterus, and on the screen the doctor sees everything that happens inside the reproductive organ. This method is considered one of the most accurate to date. An insolvent uterus scar looks like a whitish stripe (if the connective tissue prevails), retractions may be noticeable (if the scar is thin).
Treatment
To treat the scar is not accepted, the methods do not exist. If it is determined that the fertilized egg is attached to it, then abortion will be strongly recommended. In other cases, doctors will take into account the features of the scar in order to guide the pregnancy and plan the delivery technique. Rough inconsistent scars can only be removed surgically. For this, the woman will need another excision procedure, but no one will guarantee that the new scar that has formed in a couple of years will be more consistent.
According to the opinions of women and doctors, such a complication as uterine rupture is not so common in practice. But it would be irresponsible to ignore this risk. To despair a woman should not even if doctors say that she is the owner of a suture insolvent. There are clinics and individual doctors who specialize in managing pregnancies with problematic sutures in the uterus. Since there are no standards, as we found out, there is always hope.
It is only important to maintain the time interval - do not become pregnant earlier than 2 years after the previous cesarean section, follow all the recommendations of the doctor in the postoperative period. This will significantly increase the chances of a successful re-pregnancy.
About the uterine scar after cesarean section in subsequent pregnancy, see the following video.